At MedPAC’s October public meeting, the Commission discussed patterns of potentially inappropriate opioid use in Medicare’s prescription drug benefit, Part D.Opioid analgesics, a class of narcotic medications, play an important role in managing and relieving pain in patients experiencing moderate to severe pain that is not well controlled by other non-narcotic pain medications. However, they also have addictive properties and abuse of opioids in the United States is a serious problem.
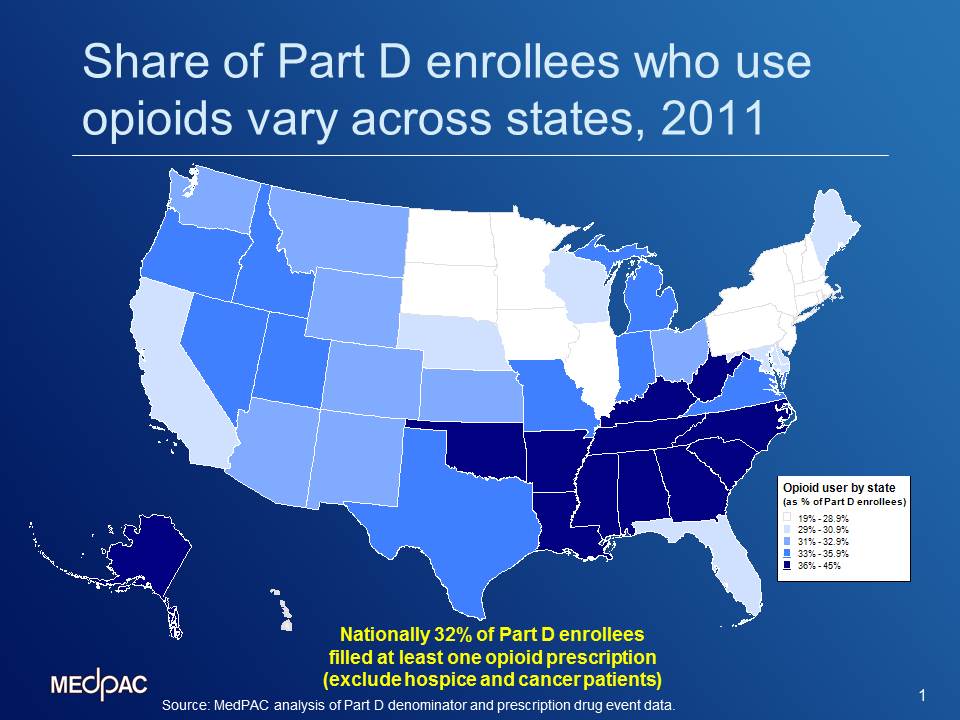
In 2011, 10 million beneficiaries, or about 32 percent of Part D enrollees filled at least one prescription for an opioid. This figure excludes about 1.5 million beneficiaries who have cancer or any hospice use throughout the year. Our analysis of the Part D data highlights wide geographic variation in opioid use among Part D enrollees. As the map above shows, the share of Part D enrollees who used opioids in 2011 varied across states, from about 20 percent in Hawaii to nearly 44 percent in Alabama, with many Southern states (Arkansas, Georgia, Kentucky, Louisiana, Oklahoma, and Tennessee) often in the low- to mid-40 percent range.
Although it is difficult to measure the extent of inappropriate use within the Part D program, AHRQ recently reported 10.6 % average annual increases in the number of inpatient stays related to opioid overuse by Medicare beneficiaries between 1993 and 2012, which raises concerns about potential inappropriate use of these medications. Even appropriate use may result in adverse health outcomes such as drug-drug interactions because many Medicare beneficiaries suffer from multiple chronic conditions, and have multiple prescriptions to manage these conditions.
Policymakers have already begun addressing the problem of opioid overuse among Part D enrollee with several initiatives. CMS has implemented a centralized data system to track potential opioid overuse cases. Plans are now required to conduct drug utilization reviews to limit the potential misuse or overuse of opioids. In 2015, prescribers will be required to enroll with the Medicare program to be able to write a Part D-eligible prescriptions. In addition, CMS plans to implement predictive analytic tool to assess fraud and abuse risk of prescribers and pharmacies based on an analysis of Part D’s prescription drug data.
The Commission also discussed other policy options that Medicare could pursue to address this problem. The slides are available here and the transcript here.
