The issue of wasteful or “low-value” health care has attracted a lot of attention in the policy community because it represents an opportunity to reduce health care spending while maintaining or even improving quality for patients. The Commission has been working on ways to measure the incidence of low-value care within Medicare. The most recent iteration of this work, which was presented at our April meeting, contributes to the evidence that Medicare beneficiaries are receiving a significant amount of low-value care.
Low-value care is the provision of a service that has little or no clinical benefit, or when the risk of harm from the service outweighs its potential benefit. In addition to increasing health care spending, low-value care may harm patients by exposing them to the risks of injury from inappropriate tests or procedures, and may lead to a cascade of additional services that contain risks but provide little or no benefit.
The Commission’s recent analysis of low-value care builds directly on work published by a team of physicians and economists in JAMA Internal Medicine in 2014 (Schwartz et al. 2014). The researchers developed 26 measures of low-value care drawn from evidence-based lists—such as the Choosing Wisely campaign, an initiative of the American Board of Internal Medicine Foundation—and the medical literature, which they applied to Medicare claims data from 2009. The authors developed two versions of each measure: a broader one with higher sensitivity (and lower specificity) and a narrower one with higher specificity (and lower sensitivity). Increasing the sensitivity of a measure captures more potentially inappropriate use, but also is more likely to misclassify some appropriate use as inappropriate. Increasing a measure’s specificity leads to less misclassification of appropriate use as inappropriate, at the expense of potentially missing some instances of inappropriate use. For example, one measure identifies inappropriate imaging for uncomplicated headache. The Choosing Wisely campaign has recommended that providers not perform imaging for uncomplicated headaches. The broader version of this measure counts all CT or MRI imaging of the head for an uncomplicated headache. The narrower version counts the same imaging studies as the broader version, but excludes beneficiaries with a diagnosis on the claim that may warrant imaging (e.g. epilepsy, cancer, or altered mental status). The narrower version therefore identifies a smaller number of services.
The Commission worked with the article’s authors to obtain their measures and methods, which we applied to 100% Medicare claims data in a later year. Consistent with their results, we show substantial use of low-value care in fee-for-service (FFS) Medicare.
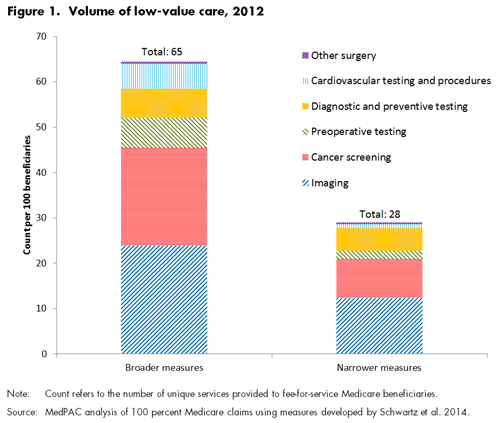
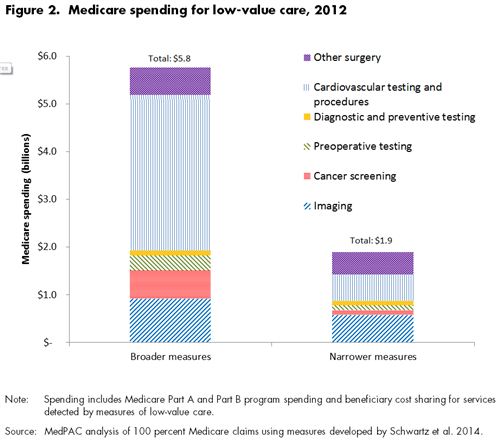
Based on the broader versions of each measure, across all measures in 2012:
- there were 65 instances of low-value care per 100 beneficiaries
- 37 percent of beneficiaries received at least one low-value service.
- Medicare spending for these services in 2012 was $5.8 billion, or 1.7 percent of total FFS Medicare spending.
Based on the narrower versions of each measure:
- there were 28 instances of low-value care per 100 beneficiaries
- 21 percent of beneficiaries received at least one low-value service.
- Total Medicare spending for these services was $1.9 billion, or 0.6 percent of total FFS Medicare spending.
The differences between the broader and narrower versions of the measures demonstrate that the amount of low-value care detected varies substantially based on the measures’ clinical specificity.
After grouping the 26 measures into six larger clinical categories, we found that imaging and cancer screening measures accounted for most of the volume of low-value care: about 70 percent of the instances of low-value care per 100 beneficiaries in both versions of the measures (Figure 1). However, cardiovascular testing and procedures and imaging accounted for most of the spending on low-value care, comprising between 60 percent and 72 percent of total spending on low-value care, depending on the versions of the measures (Figure 2).
This analysis most likely represents a very conservative estimate of the amount of low-value care in Medicare. Applying measures to Medicare claims data makes use of data available to the Commission, and allows us to examine most FFS Medicare beneficiaries. However, it is difficult to measure low-value care through claims data alone, without detailed clinical information, and it may not be possible to measure all types of low-value care with this method. In addition, our spending estimates probably understate actual spending on low-value care because they don’t include downstream services (e.g. follow-up tests and procedures) that may result from the initial low-value service.
Despite these limitations, the Commission believes that measuring low-value care is important work. The Commission has called on Medicare to tie its payments to quality of care and outcomes for many years, and the last several years have seen a pronounced shift towards value-based payments. However, most quality measurement efforts focus on the underuse or misuse of care – in other words, when patients don’t receive services that they should receive, or the services they receive are not performed correctly. Efforts to measure low-value care have been much more limited. But low value care can also harm patients and generate unnecessary beneficiary cost sharing and program spending.